Your pancreas is the gland that sends enzymes into your small intestine to break down food. It also releases hormones like insulin and glucagon into your bloodstream to help keep your blood sugar levels steady.
Pancreatic cancer begins when cells in your pancreas grow out of control and form a tumour. It often stays hidden in the early stages because symptoms can feel vague or like other less serious health issues.
You should see a doctor for pancreas cancer treatment in Singapore if you notice any of the following signs, and especially if they don’t go away:
- Yellowing of your skin or eyes (jaundice), dark urine or pale stools
- Unexplained weight loss, loss of appetite, or feeling full quickly
- Persistent upper belly or back pain, especially after eating
- Nausea, vomiting, fatigue or new-onset diabetes, especially if you don’t usually have it
How do Doctors Determine the Stage of Pancreatic Cancer?
Staging of pancreas cancer tells your care team how far the cancer has grown and where it sits in the body. To determine the stage of your pancreas cancer, the doctors will look at the tumour size, whether it touches or surrounds key blood vessels, whether lymph nodes contain cancer, and whether the cancer has spread to other organs.
This information then influences the treatment plan that is chosen for you. Clinicians often group pancreatic tumours into practical categories that guide treatment like: resectable, borderline resectable, locally advanced and metastatic.
A resectable tumour means surgeons can remove it completely, borderline resectable tumours touch nearby vessels but might be removable after treatment shrinks them. Locally advanced tumours involve major vessels and usually cannot be removed safely.
Metastatic disease means the cancer has spread beyond the pancreas and surgery is unlikely to cure it. These labels predict whether the goal is cure, long-term control, or symptom relief.
Staging relies on imaging like CT, MRI, sometimes PET and on tissue sampling by biopsy when needed. Tests also include blood checks and assessments of fitness.
Of key consideration is your general health and how well you handle surgery or chemotherapy (often called performance status). Tumour biology, such as specific gene changes, now affects choices too because it might open the door to targeted drugs. The staging step balances the technical possibility of removing the tumour with the realistic chance of benefit for you.
What is the Most Common Treatment for Pancreatic Cancer?
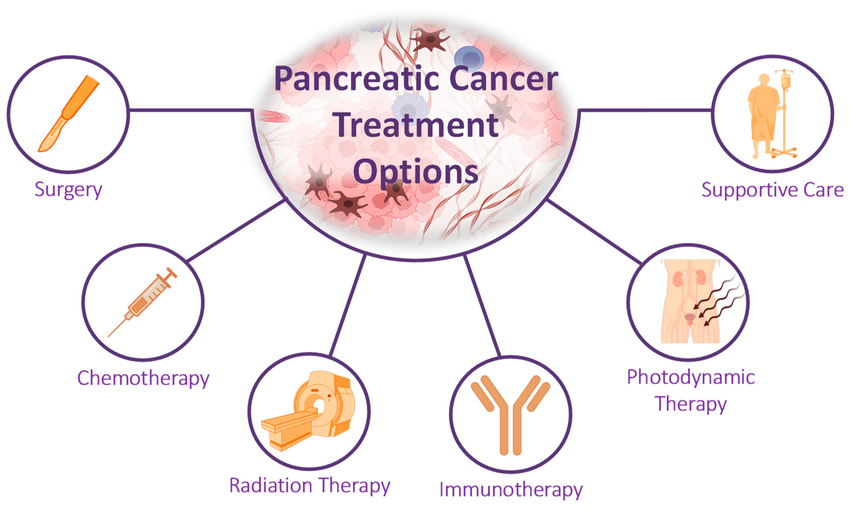
Treatment for pancreatic cancer usually falls into a few core categories. Which you get depends on the stage and your health.
The most common treatment for pancreatic cancer is surgery. The main aim of this treatment is to remove the cancer where possible and procedures typically include the Whipple (pancreaticoduodenectomy) for tumours in the head of the pancreas, distal pancreatectomy for tumours in the body or tail, and total pancreatectomy rarely used for widespread local disease.
Surgery may be suitable if you have resectable tumours and good fitness. It offers the best chance of cure when combined with further therapy. Here are a few other treatment options for you;
- Chemotherapy: Doctors use chemotherapy before surgery to shrink tumours, after surgery to reduce recurrence risk, or as the main treatment when cancer has spread. Regimens vary with one common combination for fit patients is modified FOLFIRINOX, which has shown improved survival in selected cases. Gemcitabine-based schedules remain an option for others.
- Radiation therapy: This pancreas cancer treatment method targets the tumour area and can work with chemotherapy to control local disease or ease symptoms. Teams may use short, intense courses or longer schedules depending on goals.
- Targeted therapy: If you have had tests which identified specific genetic faults, drugs that target those faults can help. For example, patients with BRCA gene changes may benefit from PARP inhibitors after initial chemotherapy. Genetic testing can identify these opportunities.
- Immunotherapy: As the name suggests, this pancreas cancer treatment approach helps the immune system fight cancer. It may be recommended if your team determines that your tumours have certain features like mismatch repair deficiency. While the role of immunotherapy is limited, it is growing.
- Palliative and supportive care: This treatment option focuses on symptoms. Specifically, it can be designed for your pain control, managing jaundice with stents, nutrition and mood. Your cancer care team can use these measures alongside any cancer-directed treatment.
As you can see, there are multiple approaches to pancreas cancer treatment which explains why some patients frequently ask; how do doctors choose treatments for pancreas cancer? Now, in an accredited facility, the decisions come from a multidisciplinary team.
That team commonly includes pancreatic surgeons, medical oncologists, clinical oncologists or radiotherapists, radiologists, pathologists and specialist nurses. The group will review your scans, biopsy results and overall health to agree the best plan.
How to Prepare for Pancreas Cancer Treatment
Proper preparation for your pancreas cancer treatment can give you more control. Your team will begin by organising tests to check heart, lung and kidney function.
They will also assess nutrition and blood sugar control. In the days leading to your treatment, you may meet a dietitian, an anaesthetist before surgery, and a nurse specialist to explain side-effect care.
If you smoke, you will need to stop to improve outcomes. If you feel weak, the team may delay treatment to strengthen you first. Practical planning also includes transport, time off work and a recovery plan at home.
When you go to appointments, you will be allowed to ask questions to address any concerns you might have about the disease or your treatment options. Here are a few sample questions you may want to ask:
- What is the goal of this treatment for me (cure, control, symptom relief)?
- What are the main side effects and how will you manage them?
- How long will treatment take and what recovery should I expect?
- Will I need a feeding tube, stent, or insulin during treatment?
- Are there clinical trials I should consider?
Use these questions to prompt clear answers about timelines, likely scans and when you will see the specialist again. Ask for written instructions on side-effect checks and emergency contact numbers.
If you care for children or work full time, tell your team. They can always help you plan support.
Wrapping Up
Pancreas cancer treatment depends on stage, tumour biology and your health. While surgery offers the best chance of cure when the tumour is removable, there are several other options you may qualify for. Prepare questions, plan practical support and ask about clinical trials or second opinions if you want them.
If you’re in Singapore, contact our clinic for a specialist review and staging assessment of your pancreas cancer treatment options. Our team offers tailored plans, genetic testing where relevant, and a nurse coordinator who guides you through tests, treatment and recovery. Call or visit us today to arrange a same-week consultation.
Dr Lee Chin Li – Lee Surgery and Endoscopy | Colorectal Surgery | Gallbladder Surgery Singapore
6 Napier Rd, #04-16 Gleneagles Medical Centre,
Singapore 258499





